The food pyramid flip

If you’ve been reading the nutrition 'news' lately, you’ve likely read a discussion or two about the new U.S. Dietary Guidelines for Americans. They’ve sparked debate across the nutrition, public health, culinary, and functional medicine communities.
I wasn’t planning on weighing in (and yes, I’m late to this party), but enough of you have asked for my perspective that this post feels warranted.
Every five years, the U.S. government releases updated Dietary Guidelines for Americans (DGAs). They’ve served as the cornerstone of U.S. nutrition policy for nearly 50 years—and through national food service programs they influence what Americans are told to eat, how food is formulated, and what gets subsidized.
Before diving in here, please know my work is not based around dietary guidelines. Personalized nutrition, metabolic resilience, food quality, and behavior change offer a far more helpful lens for personal health optimization in midlife.
What are the dietary guidelines actually designed to do?
The dietary guidelines are often discussed as though they’re clinical guidelines—but they’re not. Their intended role is to inform the following:
-
Federal nutrition programs
-
Food policy
-
Public health priorities
They’re population-level tools, not precision nutrition blueprints, and were never specifically designed for cardiometabolic risk reduction, muscle preservation, or longevity strategies in midlife.
How have the guidelines changed visually over time?
Nutrition messaging, and visuals, have evolved multiple times...
The USDA first introduced the Food Pyramid in 1992, which was actually adapted from Sweden.
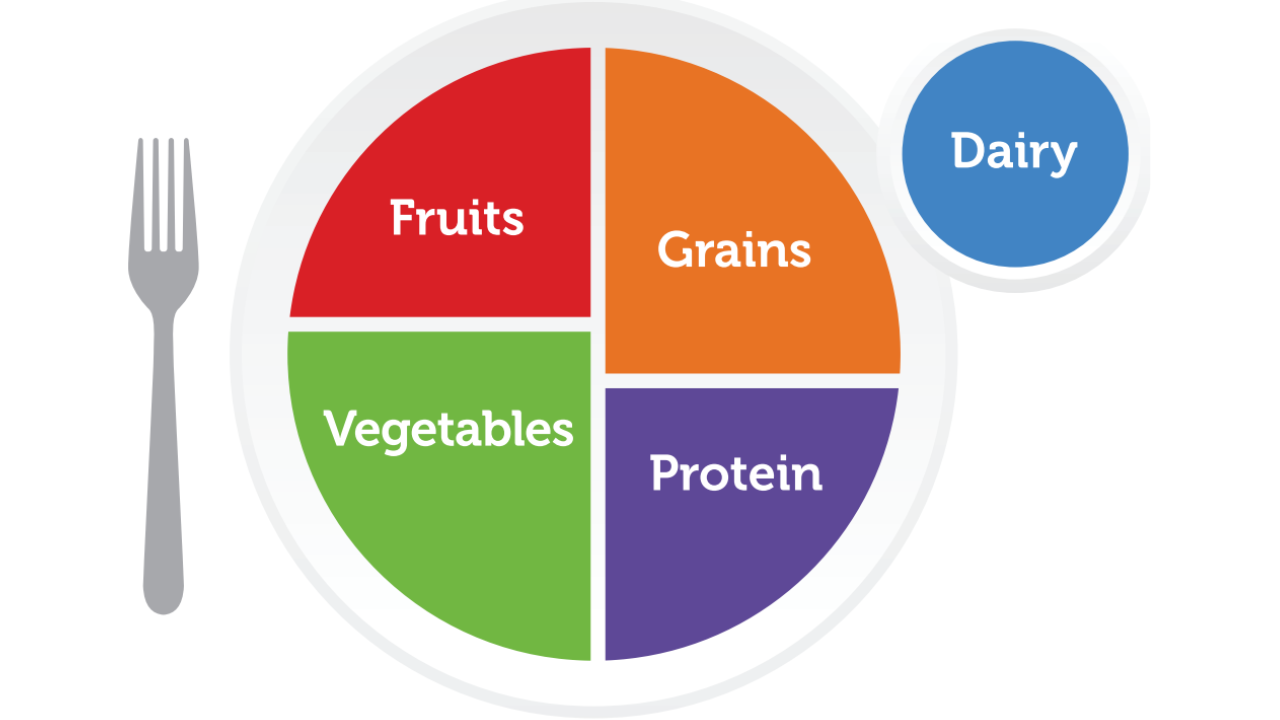
In 2011, the pyramid was replaced by MyPlate (see above). And, the latest iteration returns to a pyramid—this time inverted—adding to the headlines and confusion.
If you're in the mood for a quick ( < 1:16 second) laugh, click this link to watch the South Park spoof that actually inverted the pyramid back in 2014!
What dietary guidelines have stayed the same?
Several fundamentals remain consistent with modern nutrition science:
-
Dietary variety
-
Reduced added sugars
-
Whole, minimally processed foods
-
Nutrient density
-
Limited artificial additives
And pattern-based guidance continues to recommend:
-
Protein at each meal
-
Vegetables and fruits throughout the day
-
Whole grains in lieu of refined carbohydrates
-
Whole-food fats (meat, seafood, eggs, nuts, seeds, olives, avocado)
-
Water or unsweetened beverages
-
Limited alcohol
These remain reasonable, common sense guidelines, for a population-level baseline.
What is the most noteworthy change in the new guidelines?
The most consequential shift is the explicit acknowledgment that highly processed foods contribute to the chronic disease burden in the U.S.
For the first time, federal nutrition policy highlights the metabolic and neurobehavioral consequences of ultra-processed and ready-to-eat foods—particularly those containing emulsifiers, dyes, industrial starches, artificial sweeteners, and added sugars.
Controlled feeding trials demonstrate that ultra-processed diets drive excess calorie intake and weight gain—even when macronutrients are matched.⁴
If you're unsure how to define highly processed foods, I recommend reading Chris van Tulleken’s book Ultra-Processed People, and/or defaulting to his simple heuristic:
If your 'food' contains an ingredient that you wouldn't find in a standard home kitchen, it’s likely an ultra-processed food.
From a scientific standpoint, this acknowledgment is long overdue. And, from a policy standpoint, it’s refreshingly significant.
Ultra-processed foods are profitable, subsidized, and to-date have been deeply embedded in the U.S. food system—making this a meaningful (and political) shift.

How are protein recommendations changing?
Protein guidance has been revised to align with modern research on metabolism, aging, and muscle physiology.
The new target—1.2–1.6 g/kg (0.55–0.73 g/lb)—supports:
-
Muscle preservation
-
Appetite and satiety regulation
-
Glucose and insulin dynamics
-
Mitochondrial function
-
Frailty prevention⁵
FYI - The higher number is most relevant for adults who strength train (which should include us all BTW!).
Importantly, the revised dietary guidelines explicitly include eggs, meat, poultry, seafood, dairy, and legumes—reversing decades of protein minimization driven more by ideology than physiology.

Do these guidelines signal the end of the low-fat era?
Not necessarily, but another noteworthy change is the normalization of full-fat dairy. For decades, Americans were encouraged to choose low-fat or nonfat dairy to reduce saturated fat intake—based on the assumption that saturated fat was inherently harmful.
Large cohort studies and randomized trials now show neutral—or beneficial—associations between full-fat dairy and cardiometabolic outcomes.⁶ FYI, this is highly contingent on the individual's ability to tolerate and digest dairy.
The saturated fat cap (<10% of calories) remains in place, though evidence suggests metabolic effects depend on:
-
The food matrix
-
Metabolic context
-
The replacement nutrient
- And, of course genetics when it comes to personalized nutrition
Replacing saturated fat with refined carbohydrates worsens cardiometabolic outcomes; replacing it with whole-food sources does not.⁷

How does functional nutrition interpret the new guidelines?
From a functional and integrative perspective, the updated dietary guidelines simple reflect overdue alignment with evidence emphasizing:
-
Metabolic markers (in lieu of weight on a scale)
-
Nutrient density over ideology
-
Food quality over macronutrients
-
Protein sufficiency over deficiency
-
Whole foods over highly processed convenience foods
And, personalized nutrition simply asks better questions, for example:
-
What is your post-meal glucose response?
-
What do your ApoB, triglycerides, insulin, hs-CRP, or Lp(a) reveal about risk?
-
Which foods stabilize your energy and focus—and which destabilize it?
-
Can you comfortably go 4–6 hours between meals without feeling 'h-angry' or anxiety?
-
Are you trending toward metabolic flexibility—or relying on constant fuel?
-
Are you gaining or losing muscle in midlife?
-
How healthy is your gut, and how diverse is your microbiome?
-
Which foods lower inflammation vs. provoke it?
Population guidelines cannot answer these—and they never were intended to.
TL;DR
-
Dietary guidelines, for the general American population, are updated every 5 years
-
For the first time highly processed foods are acknowledged as drivers of chronic disease
-
Protein targets have been increased to support metabolism and aging
-
Full-fat dairy normalized; low-fat ideology fading
-
Personalized nutrition still outperforms for prevention, energy, and longevity
References
-
U.S. Department of Agriculture & U.S. Department of Health and Human Services. (2026). Dietary Guidelines for Americans 2025–2030. U.S. Government Printing Office.
-
Monteiro, C. A., Cannon, G., Levy, R. B., Moubarac, J. C., Jaime, P., Martins, A. P., Canella, D., Louzada, M. L., & Parra, D. (2018). Ultra-processed foods: What they are and how to identify them. Public Health Nutrition, 21(1), 94–101. https://doi.org/10.1017/S1368980017001348
-
Lane, M. M., Davis, J. A., Beattie, S., Gómez-Donoso, C., Loughman, A., O’Neil, A., Jacka, F., & Berk, M. (2021). Ultra-processed food and chronic non-communicable diseases: A systematic review and meta-analysis. BMJ, 374, n1957. https://doi.org/10.1136/bmj.n1957
-
Hall, K. D., Ayuketah, A., Brychta, R., Cai, H., Cassimatis, T., Chen, K. Y., Chung, S. T., Costa, E., Courville, A., Darcey, V., Fletcher, L. A., Forde, C. G., Gharib, A. M., Guo, J., Howard, R., Joseph, P. V., McGehee, S., Ouwerkerk, R., Raisinger, K., ... Zhou, M. (2019). Ultra-processed diets cause excess calorie intake and weight gain: An inpatient randomized controlled trial. Cell Metabolism, 30(1), 67–77.e3. https://doi.org/10.1016/j.cmet.2019.05.008
-
Phillips, S. M., Chevalier, S., & Leidy, H. J. (2016). Protein “requirements” beyond the RDA: Implications for optimizing health. Applied Physiology, Nutrition, and Metabolism, 41(5), 565–572. https://doi.org/10.1139/apnm-2015-0550
-
de Oliveira Otto, M. C., Mozaffarian, D., Kromhout, D., Bertoni, A. G., Sibley, C. T., Jacobs, D. R. Jr., & Nettleton, J. A. (2012). Dietary intake of saturated fat by food source and incident cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis. Circulation, 125(9), 1081–1087. https://doi.org/10.1161/CIRCULATIONAHA.111.026179
-
Ludwig, D. S., Willett, W. C., Volek, J. S., & Neuhouser, M. L. (2018). Dietary fat: From foe to friend? JAMA, 321(23), 2377–2378. https://doi.org/10.1001/jama.2019.4990
-
van Tulleken, C. (2023). Ultra-processed people: Why do we all eat stuff that isn’t food… and why can’t we stop? W. W. Norton & Company.


